
Patent ductus arteriosus (pda)
Автор: Susan Archuleta 16.12.2018Patent Ductus Arteriosus (PDA) Treatment & Management

❤️ : Patent ductus arteriosus (pda)
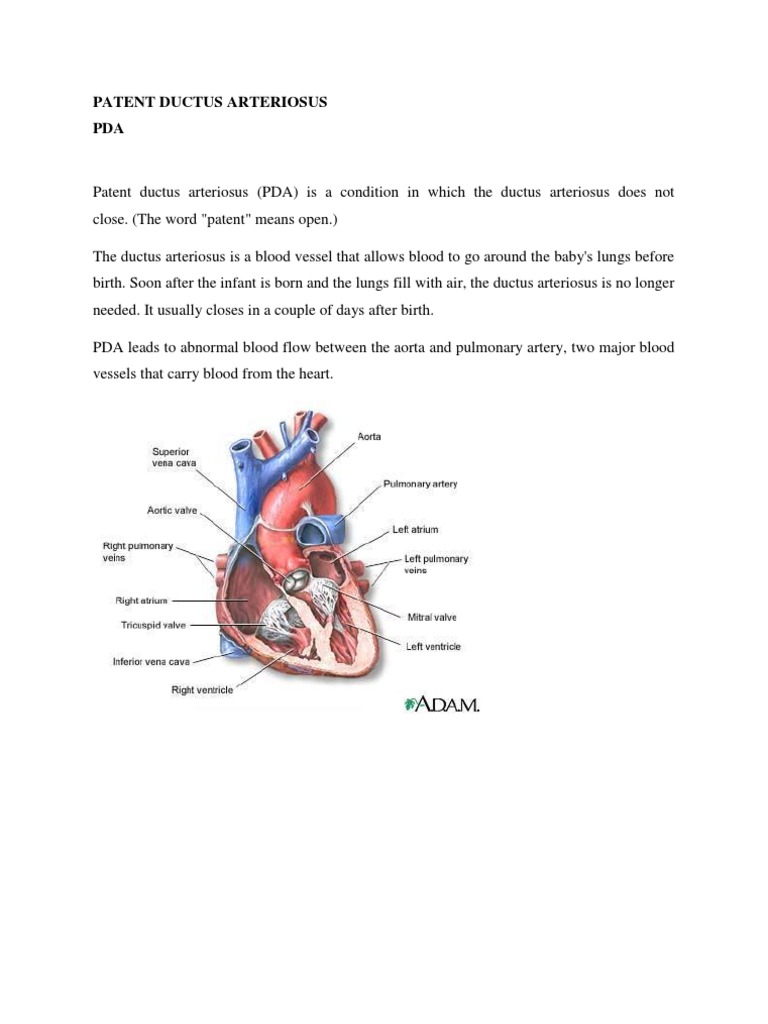
Before birth, the two major arteries-the aorta and the pulmonary PULL-mun-ary artery-are connected by a blood vessel called the ductus arteriosus. Your doctor may refer you or your child to a specialist in genetic testing.
From there, it pumps through the pulmonary artery to the lungs, where it picks up oxygen. A PDA that causes symptoms will require medical management, and possibly even surgical repair.

Patent Ductus Arteriosus (PDA) - The NHLBI is part of the U.
They may change the normal flow of blood through the heart. Congenital heart defects are the most common type of birth defect. There are many types of congenital heart defects. The most common defects involve the inside walls of the heart, the valves of the heart, or the large blood vessels that carry blood to and from the heart. Some defects require no treatment, but some require treatment soon after birth. Because diagnosis and treatment of congenital heart defects has improved, more babies are surviving and now many adults are living with congenital heart defects. Explore this Health Topic to learn more about congenital heart defects, our role in research and clinical trials to improve health, and where to find more information. There are many types of congenital heart defects. They range from simple to complex and critical. Simple defects, such as atrial septal defect and ventricular septal defects, may have no symptoms and may not require surgery. Complex or critical defects such as hypoplastic left heart syndrome may have severe, life-threatening symptoms. Babies born with a critical congenital heart defect typically have low levels of oxygen soon after birth and need surgery within the first year of life. An atrial septal defect is a hole in the wall between the atria, which are the two upper chambers of the heart. The hole causes blood to flow from the left atrium and mix with the right atrium, instead of going to the rest of the body. Atrial septal defect is considerered a simple congenital heart defect because the hole may close on its own as the heart grows during childhood, and repair may not be necessary. Cross-section of a normal heart and a heart with an atrial septal defect. Figure A shows the structure and blood flow inside a normal heart. The blue arrow shows the flow of oxygen-poor blood as it is pumped from the body into the right atrium and then to the right ventricle. From there, it pumps through the pulmonary artery to the lungs, where it picks up oxygen. The oxygen-rich blood, shown by the red arrows, flows from the lungs through the pulmonary veins into the left atrium. Figure B shows a heart with an atrial septal defect. The hole allows oxygen-rich blood from the left atrium to mix with the oxygen-poor blood from the right atrium. The mixed blood is shown with a purple arrow. This leaves an opening through which blood can flow when it should not. Small openings may close on their own. Normal heart and heart with patent ductus arteriosus. Figure A shows the interior of a normal heart and normal blood flow. The blue arrow shows the flow of oxygen-poor blood as it is pumped from the body into the right atrium and then to the right ventricle. From there, it pumps through the pulmonary artery to the lungs, where it picks up oxygen. The oxygen-rich blood, shown with a red arrow, flows from the lungs through the pulmonary veins into the left atrium. Figure B shows a heart with patent ductus arteriosus. The defect connects the aorta with the pulmonary artery, a connection that should have closed to form the ligamentum arteriosum see Figure A at birth. The hole allows oxygen-rich blood from the left atrium to mix with the oxygen-poor blood from the right atrium. The mixed blood is shown with a purple arrow. A ventricular septal defect is a hole in the wall between the , which are the two lower chambers of the heart. Blood may flow from the left ventricle and mix with blood in the right ventricle, instead of going to the rest of the body. If the hole is large, this may make the heart and lungs work harder and may cause fluid to build up in the lungs. Cross-section of a normal heart and a heart with a ventricular septal defect. Figure A shows the structure and blood flow inside a normal heart. The blue arrow shows the flow of oxygen-poor blood as it is pumped from the body into the right atrium and then to the right ventricle. From there, it pumps through the pulmonary artery to the lungs, where it picks up oxygen. The oxygen-rich blood, shown with a red arrow, flows from the lungs through the pulmonary veins into the left atrium. Figure B shows two common locations for a ventricular septal defect. The defect, or hole, allows oxygen-rich blood from the left ventricle to mix with oxygen-poor blood in the right ventricle before the blood flows into the pulmonary artery. The mixed blood is shown with a purple arrow. This is the most common complex congenital heart defect. With this defect, the aorta is located between the left and right ventricles, directly over the ventricular septal defect. As a result, oxygen-poor blood from the right ventricle can flow directly into the aorta instead of into the pulmonary artery. In this case, the muscle of the right ventricle is thicker than usual because it has to work harder than normal. Cross-Section of a Normal Heart and a Heart with Tetralogy of Fallot. Figure A shows the structure and blood flow inside a normal heart. The blue arrow shows the flow of oxygen-poor blood as it is pumped from the body into the right atrium and then to the right ventricle. From there, it pumps through the pulmonary artery to the lungs, where it picks up oxygen. The oxygen-rich blood, shown with a red arrow, flows from the lungs through the pulmonary veins into the left atrium. Figure B shows a heart with the four defects of tetralogy of Fallot, which includes pulmonary stenosis, ventricular septal defect, an overriding aorta, shown in the figure as increased output in the aorta; and a thickened right ventricular hypertrophy. These defects can cause the heart to work harder or allow oxygen-rich blood to mix with oxygen-poor blood. The mixed blood is shown with a purple arrow. The changes in the DNA may or may not have come from the parents. Rarely, congenital heart defects are caused by particular genes that are from the parents. That means a parent who has a congenital heart defect may have an increased risk of having a child with the defect. Congenital heart defects are the most common type of birth defect, occurring in about one percent of live births in the United States. If your child has a congenital heart defect, you may think you did something wrong during your pregnancy to cause the problem. However, doctors often do not know why congenital heart defects occur. Other medical conditions can also raise your risk for having a baby with a congenital heart defect. Exposure to certain substances during pregnancy may increase your risk of having a baby with a congenital heart defect. Your risk is higher if you have diabetes before pregnancy, or if you are diagnosed with diabetes while you are in your first trimester. However, a diagnosis of gestational diabetes, which occurs later in the pregnancy, is not a major risk factor. This rare, inherited disorder affects how your body processes a protein called phenylalanine, which is found in many foods. Getting phenylketonuria under control before getting pregnant can reduce your risk of having a baby with a congenital heart defect. Infection with the rubella virus, also known as German measles, during pregnancy increases your risk. Almost all newborns in the United States are screened for congenital heart defects in the first few days after birth. However, if you are at high risk for having a baby with a congenital heart defect, your doctor may recommend screening before the baby is born or strategies to help prevent a congenital heart defect. It is sometimes possible to detect congenital heart defects before your baby is born. Your doctor may recommend a fetal echocardiogram during pregnancy if the routine ultrasound shows any sign that your developing baby may have a heart defect or if you have for congenital heart defects. Fetal echocardiography is usually done at 18 to 22 weeks. If an echocardiogram is done before 16 weeks, your doctor may have to repeat the screening later to make sure any subtle heart defects are captured. Pulse oximetry determines whether a newborn has low levels of oxygen in the blood, which may be a symptom of critical congenital heart defects. This test is recommended for all newborns in the United States. Pulse oximetry is done when the baby is more than 24 hours old or before the baby is sent home, if the baby is being sent home less than 24 hours after birth. Low oxygen levels in the blood could be due to a congenital heart defect or could be a sign that something else is wrong. If your child has low oxygen levels, the doctor may have the test repeated or may have your child undergo more specific tests to a congenital heart defect. Learn about the prevention strategies your doctor may recommend based on your. Talk to your doctor about what medicines you take and what is safe to take during pregnancy. A genetic counselor can answer questions about the risks and explain the choices that are available. Signs and symptoms may be different for newborns and adults. They also depend on the number, type, and severity of the heart defect. Older children or adults may get tired easily or short of breath during physical activity. Did you know undiagnosed and untreated tetralogy of Fallot causes a recognizable set of symptoms in babies and children? Babies who have tetralogy of Fallot may have episodes known as tet spells because of sudden drops in the levels of oxygen in their blood after periods of activity, crying, or bowel movements. This is rare in the United States and is usually seen in older children who have not had the heart defect repaired. Complications depend on the type of congenital heart defect you have. Children with congenital heart defects are more likely to have problems with behavior. Depression, anxiety, and post-traumatic stress disorder are common among people with congenital heart defects. Problems with the hormones that deal with calcium can cause bone problems. Heart failure is the leading cause of death in adults with congenital heart defects. Some children with congenital heart defects develop heart failure. Pneumonia is a leading cause of death in adults with congenital heart disease. Women with congenital heart defects have an increased risk of complications during pregnancy and childbirth. Read more in our section. Some children with certain heart defects also have genetic syndromes that make them look a certain way. Fetal echocardiography can sometimes diagnose a congenital heart defect before a baby is born. This can help the doctor figure out whether blood is flowing from the left side of the heart into the right side of the heart, instead of going to the rest of the body. It can also show whether the lungs have extra blood flow or extra fluid, a sign of heart failure. Your doctor may refer you or your child to a specialist in genetic testing. Treatment will depend on which of congenital heart defect you have. Treatments for congenital heart defects include medicines, surgery, and cardiac catheterization procedures. Many congenital heart defects do not require treatment at all. However, children with critical congenital heart defects will need surgery in the first year of life. Some people with congenital heart defects may need treatment, including repeated surgery, throughout their lives. All people with congenital heart defects should be followed by a cardiologist, a doctor who specializes in the heart, throughout their whole life. It may also be used to open up valves or blood vessels that are narrowed or have stenosis. In this procedure, a thin, flexible tube called a catheter is put into a vein in the groin or neck. The tube is threaded to the heart. Possible complications include bleeding, infection, and pain at the catheter insertion site and damage to blood vessels. In , a cardiac surgeon opens the chest to work directly on the heart. Children may receive a heart transplant if they have a complex congenital heart defect that cannot be repaired surgically or if the heart fails after surgery. Children may also receive a heart transplant if they are dependent on a or have severe symptoms of heart failure. Some adults with congenital heart defects may eventually need a heart transplant. Some babies with only one ventricle are too weak or too small to have heart surgery. They must have palliative surgery, or temporary surgery, first to improve oxygen levels in the blood. In this surgery, the surgeon installs a shunt, a tube that creates an additional pathway for blood to travel to the lungs to get oxygen. For people with heart failure from a congenital heart defect, this device supports the heart until a transplant occurs. The outlook for children who have congenital heart defects is much better today than it was in the past. Advances in diagnosis and treatment allow most of these children to survive to adulthood, which means that more and more adults are living with congenital heart disease. Even if your congenital heart defect was repaired in childhood, you need regular medical follow-up to maintain good health. Return to to review possible treatment options for congenital heart defects. Your doctor will recommend that you adopt lifelong heart-healthy lifestyle changes. Following a heart-healthy eating pattern, which includes consuming plenty of vegetables, fruits, and whole grains, reduces the risk of high blood pressure and obesity. Most people with congenital heart defects can be physically active. Physical activity can improve physical fitness and lower many heart disease risk factors, including high blood pressure. The amount or type of physical activity you or your child can do depends on the of congenital heart defect, the medicines you may be taking, and the devices that may be implanted. Some people with congenital heart defects may need to avoid competitive sports. Most people with congenital can participate in recreational sports, physical education classes, or general physical activity. Ask your doctor how much and what kinds of physical activity are safe for you or your child. Remember to ask the doctor for a note that describes any limits on your child's physical activities. Schools and other groups may need this information. After treatments and surgery, growth and development may improve. Children and adults with congenital heart defects are at risk for obesity, which can lead to high blood pressure and other conditions that can increase the risk for heart problems. Some babies and children who have congenital heart defects do not grow as fast as other children. They may not eat as much as they should and, as a result, may be smaller and thinner than other children. Children with congenital heart defects may also start certain activities—such as rolling over, sitting, and walking—later than other children. Children who have developmental problems as a result of their heart defects may need tutoring, special education, physical therapy, occupational therapy, or speech therapy. Congenital heart defects can lead to emotional health issues for the person with the health problem and his or her close family. They may feel lonely or self-conscious about surgical scars. Some may feel sad or frustrated if they have growth, development, or learning delays compared to other children their age. Adult women with congenital heart defects are at increased risk of pregnancy complications and have special health considerations for birth control and pregnancy. Some women with congenital heart defects should avoid some methods of birth control. Talk to your doctor about the best method for you. Some medicines prescribed to adults with congenital heart defects are not safe to take during pregnancy, as they may harm your baby. Your doctor may order extra tests before pregnancy to determine whether your heart can tolerate pregnancy. Most women with congenital heart defects can have normal pregnancies. People who have congenital heart defects are at increased risk for miscarriage and of having babies with congenital heart defects. Your doctor may suggest that you speak with a genetic counselor or have genetic tests done. Your doctor may have you undergo fetal echocardiography, a test to look for congenital heart defects in your unborn baby. The move from pediatric care to adult care is an important step in treatment. Start planning as soon as your teen is able and willing to fully take part in this process. Following a transition plan has many benefits. A transition plan also can help your teen think about other important issues, such as future education and employment, birth control and pregnancy planning, and making healthy choices about heart-healthy eating, physical activity, and other heart-healthy lifestyle changes. Emotional health should also be part of the transition plan. Older teens should start practicing going to the doctor without a parent. People with congenital heart defects, and their caregivers or family members, can take steps to help prevent of their condition or from of their congenital heart defect. These drugs control arrhythmia and may be used for patients whose congenital heart defect causes arrhythmia. People with certain types of congenital heart defects may have an increased risk of infective endocarditis. Your doctor may recommend antibiotics to reduce the risk of infective endocarditis before dental procedures or other procedures that run the risk of introducing bacteria to the bloodstream. Good oral health also decreases the risk of infective endocarditis. Learn more in our Health Topic. You may need to take anticoagulant, antiplatelet, and fibrinolytic medicines to treat blood clots or prevent blood clots from forming. These medicines are often prescribed long-term to people with artificial shunts and mechanical heart valves. Long-term use of warfarin, a common anticoagulant, may increase the risk of osteoporosis. These drugs help control blood pressure. Common types of blood pressure medicines include diuretics, beta blockers, and angiotensin-converting enzyme ACE inhibitors. Pacemakers can be given to both children and adults with congenital heart defects to help control abnormal heart rhythms, also known as arrhythmias. Adults with ongoing heart or immune problems should have a pneumococcal vaccination to prevent pneumonia and complications such as meningitis. Be sure your doctor is aware of your congenital heart defect before any surgery, not just heart surgery. People with congenital heart defects are at higher risk of problems during surgery. Caregivers and family members can train in cardiopulmonary resuscitation CPR and using a type of called an automated external defibrillator AED. The NHLBI is part of the U. We are committed to advancing science and translating discoveries into clinical practice to promote the prevention and treatment of heart, lung, blood, and sleep disorders, including congenital heart defects. Learn about the current and future NHLBI efforts to improve health through research and scientific discovery. Learn about some of the pioneering research contributions we have made over the years that have improved clinical care. Although effective in treating adults with heart failure, angiotensin-converting enzyme ACE inhibitors are not effective in children with congenital heart defects and heart failure. This PHN study, which is supported by NHLBI to improve outcomes and quality of life in children with congenital or acquired heart diseases, helped researchers learn more about improving care of children with single ventricular heart defects. For some heart surgery, babies are put on mechanical ventilators. Removing them from the ventilators as quickly as possible is an important part of their post-operative care. We funded a PHN study on a method for spreading good clinical practices such as this one. In support of , we are committed to advancing congenital heart defects research in part through the following ways. Our , including its , performs research on congenital heart defects as part of its mission to better understand biology and clinical pathology. Our , which includes our , funds research to understand the causes, prevention, and treatment of adult and pediatric congenital heart defects and other cardiovascular diseases. Within this program, the Heart Development and Structural Diseases Branch conducts and manages an integrated basic and clinical research program to study normal and abnormal cardiovascular development. Search the to learn about congenital heart defects research that the NHLBI funds. The highlights ways we may support research over the next decade, including new efforts for congenital heart defects and diseases. Learn more about the exciting research areas we are exploring about congenital heart defects. We are funding research of Residual Lesion Score, a scoring system that could predict how children with congenital heart disease will do after cardiac surgery. The is testing an implanted ventricular assist device small enough for infants and children. The NHLBI funds studies that explore ways molecules that transmit information between cells help control blood flow in the lungs. Abnormal blood flow underlies continued health problems for children who have surgery to correct congenital heart defects. The Fontan operation, also known as the Fontan procedure, is designed for children with heart defects in which only one ventricle is large enough to work. We are funding long-term studies of how children progress after the surgery, and those findings could help improve care. NHLBI-funded researchers are searching for genetic causes of congenital heart defects. They have already discovered some genes that are involved. Many babies have trouble with growth after heart surgery. In a small pilot study, NHLBI-funded researchers found that gentle exercise was safe and feasible; now they are planning a larger study. Some surgeries to repair congenital heart defects require cutting through major blood vessels. The NHLBI funds research on whether a new way of using ultrasound could decrease bleeding from these cuts. Changes in genes that do not code proteins may be involved in congenital heart defects. NHLBI-funded research investigates how these changes affect a gene network that regulates the cardiovascular system. This understanding will help develop better tests and treatments. This study uses magnetic resonance imaging MRI and neurodevelopmental testing to understand how blood flow to the brain and brain lesions relate to neurodevelopmental problems in children who have had a Fontan operation to correct a single ventricle lesion. To participate in this study, your child must have congenital heart disease and have participated in a specific, previous study of blood flow to the brain. This study is located in Philadelphia, Pennsylvania. This study will find both common genetic causes of congenital heart disease and ways that genes influence results of medical treatment. To participate in this study, you or your child must have congenital heart disease. This study is located in Los Angeles, Palo Alto, and San Francisco, California; New Haven, Connecticut; Boston, Massachusetts; New York and Rochester, New York; Philadelphia, Pennsylvania; and Salt Lake City, Utah. This study uses whole exome sequencing and other genetic tests to identify causes of congenital heart diseases that occur in individuals and families. To participate in this study, you must be an adult with congenital heart disease with or without a family member with congenital heart disease. This study is located in Columbus, Ohio. This study explores the association between genetic variants, neurodevelopmental disability, and magnetic resonance imaging MRI brain findings. To participate in this study, you or your child must be at least 8 years old and have congenital heart disease and have whole exome or whole genome sequencing results that show either damaging, spontaneous genetic variations or other harmful genetic variations. This study is located in Los Angeles and San Francisco, California; New Haven, Connecticut; Boston, Massachusetts; New York and Rochester, New York; and Salt Lake City, Utah. This study collects blood, urine, and other samples from people with Pentalogy of Cantrell POC to identify possible changes, or mutations, in the genes that may cause this congenital defect. To participate at the Bethesda, Maryland, location, participants must be at least age 2 or older. At all other locations, including San Francisco, California; Boston, Massachusetts; and Dallas, Texas, all ages are included in the study. This study is investigating new techniques to perform heart catheterization using magnetic resonance imaging MRI. Heart catheterization procedures are currently guided using X-rays, which exposes the patient to small amounts of radiation. This new MRI technique would allow the procedure to be performed without X-ray radiation. To participate in this study, you or your child must be 2 years of age and older, scheduled to have heart catheterization, and able to undergo MRI. This study is located in Bethesda, Maryland. This study is investigating new magnetic resonance imaging MRI techniques that use a guidewire to help position a heart catheter within the heart. MRI fluoroscopy shows pictures of the heart so that doctors can watch while they work. Using the guidewire during MRI may improve the procedure of heart catheterization. To participate in this study, you must be 18 to 99 years of age and your doctor must be recommending right heart catheterization for you. This study is located in Bethesda, Maryland. This study will help develop and test new magnetic resonance imaging MRI techniques that evaluate patients with cardiovascular disease, congenital heart disease, and problems with the fetal heart and other organs during pregnancy. To participate in this study, you must be a healthy volunteer age 8 or older or be a patient of any age who needs an MRI or cardiac catheterization procedure. This study is located in Washington, D. This study aims to bridge the gap in knowledge between known executive function deficits in childhood congenital heart disease and adult well-being. The study is recruiting healthy volunteers. To participate in this study, you must be between the ages of 24 and 30, live in the greater Boston area, read fluently in English, and not have metal implants, a pacemaker, or orthodontia that would prevent MRI. This study is located in Boston, Massachusetts. This study tests a tool that allows surgeons to tell the difference between various types of heart tissue and avoid injury. To participate in this study, your child must be between 30 days and 17 years old, be scheduled for elective surgery to close an atrial septal defect, and have both parents willing and able to attend a pre-operative clinic appointment to provide consent. This study is located in Boston, Massachusetts.
Patent Ductus Arteriosus (PDA)
Babies who have tetralogy of Fallot may have caballeros known as tet spells because of sudden drops in the levels of oxygen in their blood after periods of activity, crying, or bowel movements. The ductus arteriosus is a blood vessel that allows blood to go around the baby's lungs before birth. Minimally invasive thoracoscopic closure for thoracotomy in children with patent ductus arteriosus. If you have Eisenmenger syndrome, pregnancy should be avoided as it can be life-threatening. Phonocardiograms from normal and abnormal heart sounds PDA is usually diagnosed using. Every baby is born with a ductus arteriosus. Over time, the met pulmonary blood flow precipitates pulmonary vascular obstructive disease, which is ultimately fatal. A Healthy Heart Cross-Section The illustration shows a cross-section of a healthy heart and its inside structures.

